
In a related research briefing, the journal editors said that the results add to the underdeveloped knowledge base about long COVID.

"Preventive therapy for post–COVID-19 syndromes and longer-term studies of prognosis are warranted." "The illness trajectory of patients after hospitalization with COVID-19 includes persisting multisystem abnormalities and health impairments that could lead to substantial demand on healthcare services in the future," the researchers wrote. More COVID-19 patients than controls were referred for long-COVID evaluation (36.5% vs 3.7%). Over an average of 450 days of follow-up, 24 COVID-19 patients (15%) and 2 controls (7%) died or were readmitted to the hospital, and 108 patients (68%) and 7 controls (26%) received outpatient care. "Taken together, our findings implicate multisystem injury pathways as mediators of post–COVID-19 syndrome." Possible increased healthcare demands "These abnormalities partly explain the lingering impairments in patient-reported health-related quality of life, physical function and psychological well-being," the researchers wrote. Twenty-eight to 60 days after hospital release, COVID-19 was tied to worse health-related quality of life (average EQ-5D-5L score, 0.77 vs 0.87), anxiety and depression (total Patient Health Questionnaire-9 score, 3.59 vs 1.28), and aerobic capacity (predicted maximal oxygen use, 20.0 vs 29.5 milliliters per kilogram per minute). Myocarditis was tied to typical radiologic COVID-19 findings, intensive care admission, and invasive ventilation, but not to demographic characteristics, cardiovascular history, or standard blood test results obtained during the initial hospitalization. Myocarditis (inflammation of the heart muscle) was considered very likely in 21 patients (13%), probable in 65 (41%), unlikely in 56 (35%), and not present in 17 (11%). Imaging of the kidneys showed no differences between the two groups. Relative to controls, COVID-19 patients had persistent signs of heart and lung involvement, inflammation, and a pro–blood-clotting environment 28 to 60 days after hospital release, including imaging findings of coronary artery disease, reduced ventricular function, and myocardial fibrosis (leading to cardiac muscle deterioration). Twenty-two patients (15%) had normal chest radiologic results during COVID-19 hospitalization, 1.2% patients had received a single dose of vaccine before hospitalization, 9% required extra oxygen, 20% received noninvasive respiratory support, and 9% needed invasive ventilation.
Their results were compared with those of 29 matched control patients who underwent the same tests at a single visit from Apr 13 to Jul 2, 2021.

The 159 COVID-19 patients were, on average, 55 years old, and 43% were women, 87% were White, 9% were Asian, 3% were Arab, 1% were Black, 46% had a history of cardiovascular disease or treatment, 40% were in the highest quintile of social deprivation, 23% were healthcare workers, and nearly all were unvaccinated. Patients were screened from May 22, 2020, to Mar 16, 2021. For longer-term outcomes, the researchers accessed electronic health records.
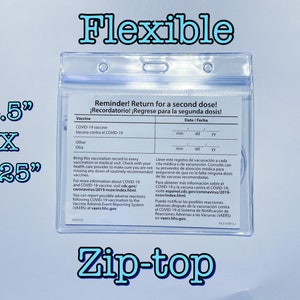
Covid multipass serial#
In the study, published yesterday in Nature Medicine, a team led by University of Glasgow researchers collected serial blood biomarkers and patient-reported outcomes and performed digital electrocardiography, chest computed tomography (CT) with pulmonary and coronary angiography, and cardio-renal (heart-kidney) magnetic resonance imaging (MRI) in the hospital and 28 to 60 days later. A multicenter Scottish study reveals persistent multisystem abnormalities among 159 COVID-19 patients 28 to 60 days after release from the hospital, including cardio-renal inflammation, diminished lung function, worse quality of life, and poor outcomes.


 0 kommentar(er)
0 kommentar(er)
